When is ECHO needed?

When is ECHO needed?
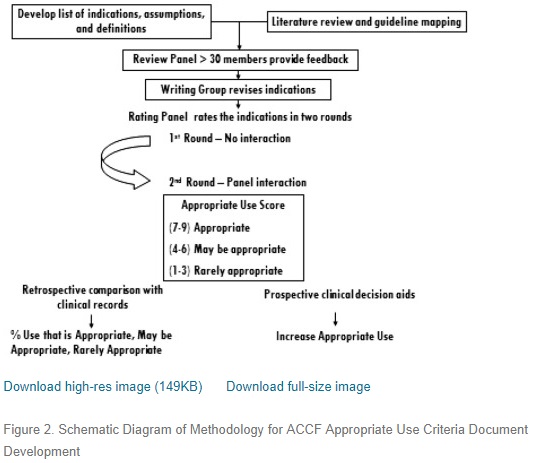
In 2007, a guideline of appropriateness of ECHO as a tool for assessment of a sets of specific conditions was introduced. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 Appropriateness Criteria for Transthoracic and Transesophageal Echocardiography.
2011- ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/ SCCT/SCMR 2011 Appropriate Use Criteria for
Echocardiography
Initially, it goes with an appropriateness scoring which now is evolved into Appropriateness Use Care (AUC). And not only that, if you see the evolution, is the expansion of this initiative from imaging to devices and procedures including coronary revascularization, diagnostic catheterization, implanted cardiac defibrillators, and cardiac resynchronization devices.
—
Score 7 to 9
Appropriate test for specific indication (test is generally acceptable and is a reasonable approach for the indication
Median Score 7 to 9: Appropriate Care
An appropriate option for management of patients in this population due to benefits generally outweighing risks; effective option for individual care plans although not always necessary, depending on physician judgment and patient specific preferences (i.e., procedure is generally acceptable and is generally reasonable for the indication)
—
Score 4 to 6
Uncertain for specific indication (test may be generally acceptable and may be a reasonable approach for the indication). (Uncertainty also implies that more research and/or patient information
is needed to classify the indication definitively.)
Median Score 4 to 6: May be Appropriate Care
At times, an appropriate option for management of patients in this population due to variable evidence or agreement regarding the benefits/risks ratio, potential benefit based on practice experience in the absence of evidence, and/or variability in the population; effectiveness for individual care must be determined by a patient’s physician in consultation with the patient based on additional clinical variables and judgment along with patient preferences (i.e., procedure may be acceptable and may be reasonable for the indication).
—
Score 1 to 3
Inappropriate test for that indication (test is not generally acceptable and is not a reasonable approach for the indication).
Median Score 1 to 3: Rarely Appropriate Care
Rarely an appropriate option for management of patients in this population due to the lack of a clear benefit/risk advantage; rarely an effective option for individual care plans; exceptions should have documentation of the clinical reasons for proceeding with this care option (i.e., procedure is not generally acceptable and is not generally reasonable for the indication).
The appropriateness criteria in the report provide an estimate of the reasonableness of the use of TTE/TEE for the particular clinical scenario.
But I would like to highlight only the inappropriate indications (those of scoring 1- 3)
Indications,
These were from 2007
4.Routine (yearly) evaluation of asymptomatic patients with corrected ASD, VSD, or PDA more than 1 year after successful correction
5.Patients who have isolated APC or PVC without other evidence of heart disease
7. Evaluation of LV function with prior ventricular function evaluation within the past year with normal function (such as prior echocardiogram, LV gram, SPECT, cardiac MRI) in patients in whom there has been no change in clinical status)
15. Initial evaluation of patient with suspected pulmonary embolism in order to establish diagnosis
19. Routine (yearly) re-evaluation of mitral valve prolapse in patients with no or mild MR and no change in clinical status
21. Routine (yearly) re-evaluation of an asymptomatic patient with mild native AS or mild-moderate native MS and no change in clinical status
22. Routine (yearly) re-evaluation of native valvular regurgitation in an asymptomatic patient with mild regurgitation, no change in clinical status, and normal LV size
29. Routine (yearly) evaluation of a patient with a prosthetic valve in whom there is no suspicion of valvular dysfunction and no change in clinical status
32. Evaluation of native and/or prosthetic valves in patients with transient fever but without evidence of bacteremia or new murmur
39. Routine evaluation of patients with systemic hypertension without suspected hypertensive heart disease
40. Re-evaluation of a patient with known hypertensive heart disease without a change in clinical status
42. Routine (yearly) re-evaluation of patients with heart failure (systolic or diastolic) in whom there is no change in clinical status
47. Routine (yearly) evaluation of hypertrophic cardiomyopathy in a patient with no change in clinical status
58. Evaluation of a patient with atrial fibrillation/flutter for left atrial thrombus or spontaneous contrast when a decision has been made to anticoagulate and not to perform cardioversion.
2011 – ECHO plus stress ECHO
20. Assessment of volume status in a critically ill patient U (5)
27.Respiratory failure or hypoxemia when a noncardiac etiology of respiratory failure has been established
28. Suspected pulmonary embolism in order to establish diagnosis
30. Routine surveillance of prior pulmonary embolism with normal right ventricular function
and pulmonary artery systolic pressure
33. Routine evaluation in the setting of mild chest trauma with no electrocardiographic changes or biomarker elevation
35. Initial evaluation when there are no other symptoms or signs of valvular or structural heart disease
36. Re-evaluation in a patient without valvular disease on prior echocardiogram and no change in
clinical status or cardiac exam
56. Routine surveillance of uncomplicated infective endocarditis when no change in management is
contemplated
60. Routine surveillance of known small pericardial effusion with no change in clinical status
88. Routine surveillance (<1 y) of known cardiomyopathy without a change in clinical status or cardiac exam
95-97- some survelliance of reasessement of repaired congenital heart.
107. To diagnose infective endocarditis with a low pretest probability (e.g., transient fever, known
alternative source of infection, or negative blood cultures/atypical pathogen for endocarditis)
General Patient Populations With Stress Echocardiography
124. Low global CAD risk I (1)
125. Intermediate global CAD risk ECG interpretable I (2)
126. Intermediate global CAD risk ECG uninterpretable U (5)
127. High global CAD risk U (5)
Asymptomatic: Prior Evidence of Subclinical Disease With Stress Echocardiography
136. Coronary calcium Agatston score <100 I (2)
137. Low to intermediate global CAD risk Coronary calcium Agatston score between 100 and 400 U (5)
138. High global CAD risk Coronary calcium Agatston score between 100 and 400 U (6)
139. Coronary calcium Agatston score >400 A (7)
140. Abnormal carotid intimal medial thickness ($0.9 mm and/or the presence of plaque encroaching into the arterial lumen) U (5)
U is undetermined
Asymptomatic or Stable Symptoms With Stress Echocardiography Normal Prior Stress Imaging Study
142. Low global CAD risk Last stress imaging study <2 y ago I (1)
143. Low global CAD risk Last stress imaging study >2 y ago I (2)
144. Intermediate to high global CAD risk Last stress imaging study <2 y ago I (2)
145. Intermediate to high global CAD risk Last stress imaging study >2 y ago U (4)
It goes further to ischaemic equivalent

Evolving into this
Further reading
- Appropriate Use Criteria for Echocardiography: Evolving Applications in the Era of Value-Based Healthcare
-
Appropriate Use of Cardiovascular Technology: 2013 ACCF Appropriate Use Criteria Methodology Update: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force
https://doi.org/10.1016/j.jacc.2013.01.025






One day I’ll read and understand this, but not today or the next month or… Hahaha
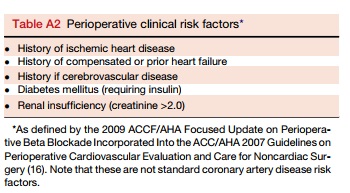
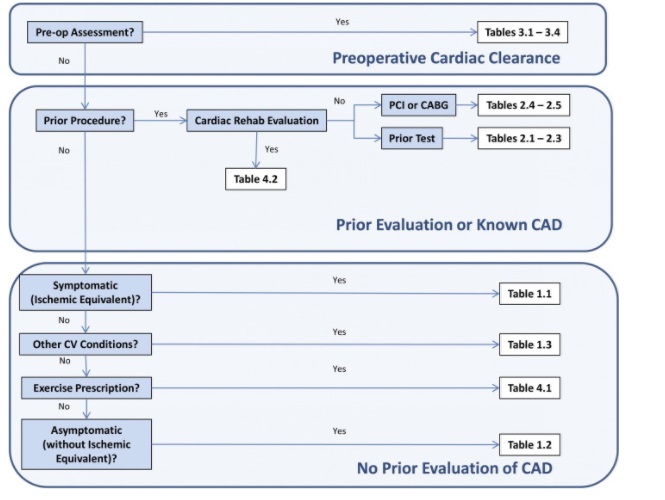
You may want to refer to the 2014 AHA and the 2014 ESC guidelines on cardiac assessment for non-cardiac surgery. It appears more simplified and applicable.
Muhammad Amir Ayub
March 4, 2018 at 11:53 pm